A Community of Healing
Arriving in southern Uganda in 2002, Teachers College psychologist Lena Verdeli knew she had her work cut out for her. The country had endured a brutal civil war and was still in the midst of a devastating AIDS epidemic. Vast numbers of people in the northern regions were living in internally displaced persons camps. A qualitative assessment of mental-health needs by Johns Hopkins University showed that many adults were so paralyzed by yo’kwekyawa and okwekubazida – self-hatred and self-pity – that they were neglecting their families and cutting themselves off from community resources.
Verdeli, Director of TC’s Global Mental Health Lab, thought these states of mind sounded strikingly like depression, but she worried about “medicalizing” extreme suffering. After all, who wouldn’t be depressed living under such adverse conditions? Still, she was encouraged by a field report from her colleague, Paul Bolton, a Johns Hopkins public health researcher, indicating that Ugandans themselves recognized they had a problem and were eagerly seeking help.
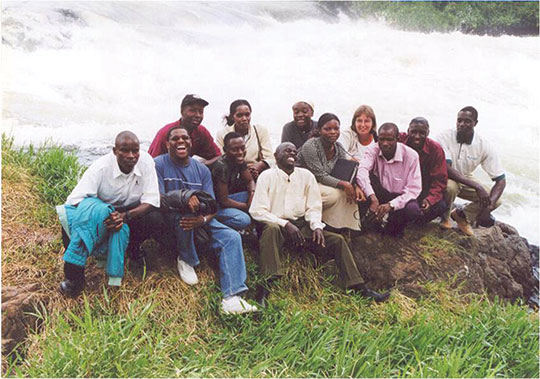
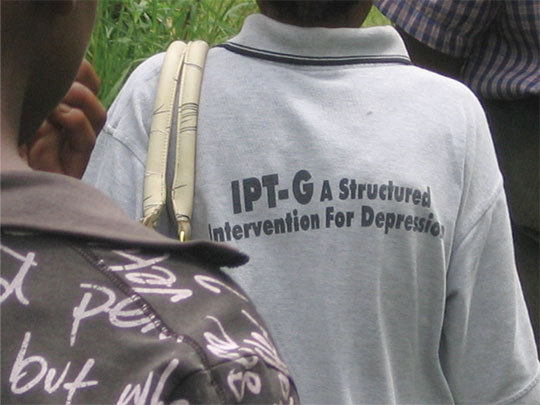
With few doctors available and no funds to provide medication, Bolton had recruited Verdeli to collaborate in a clinical trial of interpersonal psychotherapy (IPT), a time-limited treatment for depression, with standardized steps and inclusion criteria, codeveloped by her mentor, Columbia University psychologist and epidemiologist Myrna Weissman. Under an agreement with the nongovernmental organization World Vision, Verdeli and a colleague, Kathleen Clougherty, would train African mental health professionals employed by World Vision to lead group therapy sessions among the villagers.
Yet, almost as soon as they stepped off the plane, Verdeli and Clougherty learned from Bolton that World Vision had decided it could not spare its personnel. Instead, Verdeli and Clougherty would be working with the mental health workers’ younger brothers and sisters – people who had no psychological training at all.
“Kathy and I just looked at each other and said, ‘Now we are here, why not?’” Verdeli says.
In the end, the raw recruits turned out to be a blessing in disguise. Since they came from the same communities as the study participants, they gave valuable input about the local culture, where people seemed to view themselves primarily as community and family members rather than as individuals.
“There is an old African saying, ‘People are people within people,’” Verdeli says. “It means that people are defined by other people, by a mutual and endless reflection of themselves in their community and group that constantly shapes and reshapes individual identity.”
Tossing aside their training guides, Verdeli and Clougherty asked their trainees open-ended questions in order to develop a culturally relevant context for understanding Uganda’s malaise.
For example, Verdeli says, IPT theory identifies four categories of depression triggers: the death of a loved one; covert and overt disputes; life transitions such as job loss or divorce; and interpersonal deficits such as longstanding difficulties in initiating and maintaining relationships. However, during the discussions the trainees gave them examples that fit into the first three categories but not the fourth.
“They basically told us, ‘We don’t have that problem here, because we do everything in groups,’” Verdeli says.
The trainees also provided valuable insights in conducting role-play exercises designed to help people explore acceptable ways of becoming “unstuck” from oppressive situations. Sometimes they described solutions that might have eluded or even alienated someone with Western values.
For example, when a woman in Uganda discovers she cannot conceive, an acceptable option might be to ask a friend or a relative to marry her husband and give one of the resulting children to her to parent as her own. Or, when a man with AIDS insists that his wife have unprotected sex with him, she might ask an older member of her husband’s family to act as her advocate, and thereby avoid the ostracism that will follow from resisting and being sent back to her parents’ home.
A randomized, controlled trial of Verdeli’s IPT program in southern Uganda was conducted. Participants who received the treatment reported an 80 percent reduction in prevalence of depression at the end of the trial. World Vision hired the trainees, who went on to treat – and train others to treat – some 6,000 people. Ironically, World Vision ultimately closed the program precisely because it was so successful (passing it on to volunteers) and turned its attention elsewhere – a common occurrence in humanitarian development agencies.
Following the success of IPT in southern Uganda, Verdeli and Clougherty were asked by another NGO, War Child, to adapt IPT for children in internally displaced persons camps in northern Uganda. Many of the children had previously been abducted by rebels in the Lord’s Resistance Army, a militant cult accused of widespread human rights abuses. There were important differences in these populations. For example, unlike the adults in the south, many of the children had interpersonal deficits as a result of their traumatic developmental histories. “The kids had grown up without attachments, and sometimes with very limited language,” Verdeli says. “Sometimes their objects of attachment were the rebels themselves. The kids were very confused because some of the rebels were actually affectionate with them.” An IPT adaptation for these children was compared with an existing, play-therapy intervention and was shown to be more effective in improving depression.
Verdeli has applied lessons learned from Uganda to her work elsewhere. For example, in order to ensure sustainability, her projects in Goa and Haiti are built around partnerships with local health care centers, government agencies and universities. Meanwhile, she and others are building the case globally for improving the treatment of depression in under-resourced areas. That’s important, because as infectious diseases are increasingly brought under control, depression is emerging as the condition with the greatest impact worldwide, as measured by financial cost, death and other factors. The World Health Organization reports that 75 percent of the world’s neuropsychiatric disorders occur in lower-income countries.
“International donors and agencies have known for a long time that depression is incredibly disabling,” Verdeli says, but they’ve focused on poverty, disease and other conditions that breed it. “Since our team and others showed through studies that distress can be significantly alleviated even in the context of extreme poverty, international agencies have started paying more attention.”
Teachers College and Columbia are capitalizing on this momentum, collaborating with the New York State Psychiatric Institute and Columbia’s Mailman School of Public Health to create a Global Mental Health program that offers two different master’s degree programs – one based at Mailman that emphasizes epidemiology and policy, and one at TC that emphasizes mental health assessment and treatment.
“Global mental health is going to be a major source of innovation, because people in under-resourced areas have to think out of the box to deal with the shortages,” Verdeli says. For example, in Haiti, community health workers do regular checkups with people afflicted with a number of health conditions – an approach Verdeli would love to see adopted in the United States: “Let’s not forget we have a lot of under-resourced communities in our own backyard.”
Published Friday, Dec. 7, 2012